Z Lamich, A Yahia*, M Elalaoui Elhanafi, K Maani and A Abkari
Pediatric Resident, Department of Pediatric, Morocco
*Corresponding Author: A Yahia, Pediatric Resident, Department of Pediatric, Morocco.
Received: February 19, 2024; Published: March 11, 2024
Citation: A Yahia., et al. “Torticollis Revealing an Unusual Location of Ewing's Sarcoma in Children”. Acta Scientific Paediatrics 7.4 (2024): 10-12.
Torticollis is a common symptom in children. The etiologies are multiple and most often benign but sometimes it can reveal a serious disease in particularly a malignant tumor pathology [10].
The fourth edition of the WHO Classification of Tumors of Soft Tissue and Bone defines Ewing sarcoma as small round cell sarcoma with characteristic molecular findings and varying degrees of neuroectodermal differentiation. It is characterized in most cases by recurrent balanced translocations between the EWSR1 gene on chromosome 22 and genes belonging to the ETS family of transcription factors [1].
Objective: illustrate the example of a torticollis of unusual evolution related to a malignant tumor of the cervical spine
We report the case of an eight year old female child with No particular medical history, hospitalized with torticollis evolving for 3 months, resistant to analgesic and anti-inflammatory treatment monoparesis in a context of fever with night sweats and weight loss.
The clinical examination had found a patient with jugulo-carotid tumefaction left 4 cm X 6 cm, hard, fixed in relation to the deep plane, without inflammatory signs in gaze, decreased left upper extremity muscle strength with enophthalmia and ptosis.
The MRI demonstrates a lesional process of the left lateral cervical region with epidural endo-canal extension extended over 10 cm with an anomaly of the C5 body signal+ A blood clot.
The biopsy of the mass demonstrates the presence of round cells on histological examination and the immuno-histochemical study is in favor of vertebral Ewing’s sarcoma.
The treatment indicated is chemotherapy according to the Euro-Ewing 99 protocol (6 courses of VIDE) followed by 6 radiotherapy sessions with a good clinical evolution. The Post-chemo control MRI showed a disappearance of the cervical mass with total decompression of the bone marrow. We opted for maintenance chemotherapy with radiotherapy since there is no longer any indication for surgery.
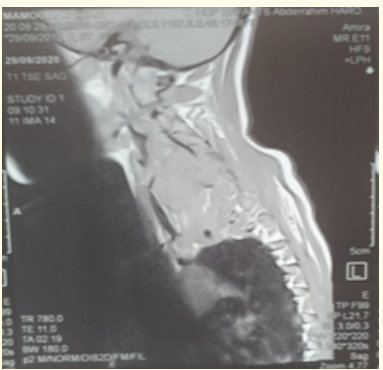
Figure 1: Image of Ewing's sarcoma before chemotherapy.
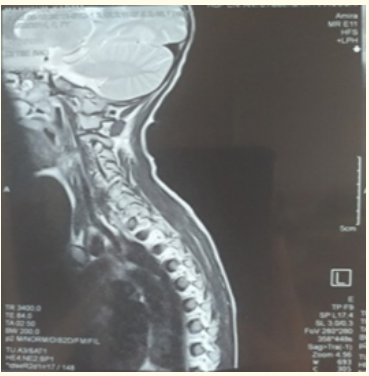
Figure 2: Aspect normal après chimiothérapie.
Ewing’s sarcoma (ES) is a locally aggressive bone malignancy that is seen more frequently in males. It is considered the second most common primary malignant bone tumor in children and adolescents after osteosarcomas. ES is most frequently detected in the long bones. Primary SE of the neck region is very rare, including only 1% to 4% of all cases of SE [9].
Most patients with Ewing’s sarcoma present with tumour-related symptoms, such as pain or a mass. In the literature The most common clinical presentation of SE is a pain syndrome and muscle weakness proportional to the location of the tumor [1,2].
The first step in the assessment phase should be imaging of the suspected tumour, preferably by MRI, encompassing the entire involved bone or compartment, the biopsy confirms the diagnosis of Ewing’s sarcoma in the various studies as in our patient. A complete staging assessment includes a CT scan of the chest to detect pulmonary metastases, bone scintigraphy to detect bony metastases, and bone marrow aspirate and biopsy. Each of these techniques has limited sensitivity and specificity and is constantly evolving, the fraction of patients with detectable metastases at diagnosis has remained fairly stable at 20-25% [2].
Advanced imaging is performed to more precisely define the extent of the primary tumor and assess its location relative to the adjacent bones, muscles, joints, blood vessels, and nerves. A multiinstitutional study of 387 patients that included both children and adults found that magnetic resonance imaging (MRI) and computed imaging is performed to detect the presence of metastatic disease. In the case of Ewing sarcoma, approximately 25% of patients have detectable metastatic disease at presentation most commonly in the lungs (approximately 50%), followed by bone (approximately 25%) and bone marrow (approximately 20%) [10].
The standard therapeutic approach consists of neoadjuvant/induction chemotherapy (neoCT), followed by local treatment (surgery and/or radiotherapy) associated with consolidation/maintenance chemotherapy adapted to the risk [4].
IESS-1 (the Intergroup ES Study), which included 331 patients, compared the prognosis of patients that were treated with the VAC regimen (VCR, ACT-D, and CPM) and that of patients that were administered the VAC + DOX (VACD) regimen. As a result, it was found that the addition of DOX had a beneficial effect on patient survival. Patients treated with the VAC regimen alone, the VAC regimen and whole lung irradiation, or the VACD regimen alone exhibited 5-year disease free survival rates of 24, 44, and 60%, respectively. IESSII, which included 293 patients, reported that patients that were treated with an intensified VACD regimen displayed a 5-year disease-free survival rate of 68 %, where as that of the patients treated with a moderate dose VACD regimen was 48% [3].
The current standard of care for the delivery of radiation therapy includes involved field radiation with limited margin The RT target volume includes the prechemotherapy extent of disease with limited margin to an intermediate dose (45 Gy) and boosting gross residual after chemotherapy where there was soft-tissue response at pushing borders and all initially involved bone (55.8 Gy). Standard RT doses for Ewing sarcoma are between 50 and 60 Gy [4].
The combination therapies may enhance the efficacy and decrease the resistance. RTK inhibitors have shown synergistic effects with chemotherapeutic agents. mTOR inhibitors have been more effective in combination with other agents, such as IGF1R inhibitors [6].
The Oncolytic viruses (OV) can selectively infect and kill tumor cells, while sparing normal tissues. Phase I/II clinical trials using OV in carcinoma patients demonstrated remarkable safety profiles and notable clinical effects. A systemic delivery of vesicular stomatitis virus (VSVΔM51) resulted in a significant decrease of tumor burden in ES bearing mice, and tumor-specific killing of resistant ES cells [7].
Surgical options: En-bloc excision at the occipitocervical junction presents a tremendous technical challenge. Liu et al. utilized a that 3-D printed, customized self-stabilizing artificial vertebral body to treat primary Ewing’s sarcoma involving the C2 vertebra in a 12-year-old male following complete C2 excision. However, there are limited data regarding the long-term efficacy of such implants, Although the axial location of a Ewing’s sarcoma is a poor prognostic factor, the combined use of chemotherapy and radiotherapy has improved the overall prognosis/survival in the past two decades [5,9].
Neck pain and torticollis are common in children and require investigation. However, the persistence of the symptoms imposes a meticulous approach in search of an etiology and particularly a malignant process [4].
The treatment of ES relies on a multidisciplinary approach that couples risk-adapted chemotherapy and local therapy (surgery, radiation therapy, or both) to maximize the chance of cure and minimize the risk of long-term sequelae [4,6].
The mutual interest of researchers advanced the understanding of ES oncogenesis and genetic susceptibility for developing ES. Since the discovery and characterization of the causal translocation involving the EWS gene on chromosome 22 and an ETS-type gene.
Researchers have evaluated genes modulated by the chimeric fusion, oncogene EWS-FLI1 (and similar fusion genes) that could serve as therapeutic targets. Indeed, although targeting EWS-FLI1 directly reverses the malignant phenotype, this finding has not been translated into clinical practice [8].
Copyright: © 2024 A Yahia., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.