Chakradhar Maddela*
Consultant Neonatologist and Echocardiologist, Manikrishna Hospital, Metpally, India
*Corresponding Author: Chakradhar Maddela, Consultant Neonatologist and Echocardiologist, Manikrishna Hospital, Metpally, India.
Received: November 14, 2022; Published: January 26, 2023
Citation: Chakradhar Maddela. “A Simple Practicable Prediction Tool for Sick Children: Surcu5 - A Conceptual Research Framework”. Acta Scientific Paediatrics 6.2 (2023): 32-35.
Clinical risk scores are essential in clinical practice for disease stratification and prognostication. This is especially true for under five sick children. Sick children have narrow margin of safety between disease manifestation and clinical deterioration and its associated high mortality. Many available clinical scores are essential but complex to practice due to number of parameters and scoring system used. Hence, a simple and practicable risk tool comprising few parameters and easy scoring system is mandatory for daily paediatric practice especially during surge of endemic diseases. We conceptually framed a simple and practicable risk tool “SURCU5” for paediatric purpose.
Keywords: Tool; Sick Children; Surcu5
AKI: Acute Kidney Injury; BTS: British Thoracic Society; CRT: Capillary Refill Time; ESR: Emergency Service Room; IP: Inpatient; OP: Outpatient; PICU: Paediatric Intensive Care Unit; RR: Respiratory Rate; UNICEF: United Nations International Children’s Emergency Fund; U5MR: Under-Five Mortality Rate; WHO: World Health Organization
A simple, practicable, easily memorable risk score with less clinical parameters is very much needed for clinical practice. The risk score should identify and grade the sick children, assist in deciding where to station them in delivering health care and to initiate appropriate risk-based management. Many available clinical risk scores are complex with number of parameters and not easy to practice without device or app assistance. This is so true in a busy paediatric out patient (OP) or during patient first contact at paediatric emergency department especially during seasonal surge of endemic diseases or epidemics in tropical countries like India.
We faced challenges in clinical practice while deciding correctly which sick child needs hospitalisation, if yes - where to station them at health care facility? and what type of medical intervention is needed?. It is hard to decide the allocation of clinical resources like beds, man and machine without a clinical tool especially when they are limited and bed occupancy and referrals from outside are high as seen during surge in endemic diseases like dengue fever, other viral fevers, respiratory tract infections, bronchial asthma, gastroenteritis, malaria etc. in tropical countries like India.
The above clinical situation stimulated me to search online and offline for available simple clinical risk scores which can fit and solve above problem at our centre. “CURB-65” clinical risk score is a simple risk score tool intended for clinical use in elderly patients by British Thoracic Society (BTS) [1]. It is well evaluated and practiced widely in clinical medicine. I had modified the adult clinical scoring system “CURB 65” and framed with practicable simple clinical parameters for paediatric purpose based on my clinical experience and observations in the past.
The proposed paediatric clinical risk score included risk parameters like altered sensorium, oliguria or anuria, respiratory rate (RR), delayed capillary refill time (CRT) >3seconds and one to under-fives high risk group. This score is simple and can be used both by doctors and nurses at patient first contact or in outpatient department during busy paediatric consultation hours so that all at risk children quickly identified, triaged and managed properly.
This concept helped us in allocating the available resources at our facility to identify, station (as OP at home care, hospitalization and admission in the paediatric ward and PICU/Paediatric Emergency Service Room admission) and manage the sick patients based on our framed risk tool. This had reduced the under fives mortality to almost zero figures at our health care facility, Manikrishna Hospital, Metpally, India. This clinical score abbreviated as “SURCU5”. This score includes five simple, clinical parameters for risk scoring. A normal parameter was given score zero and scored one when parameter noticed abnormal. Total maximum score is 5 and the minimum is zero.
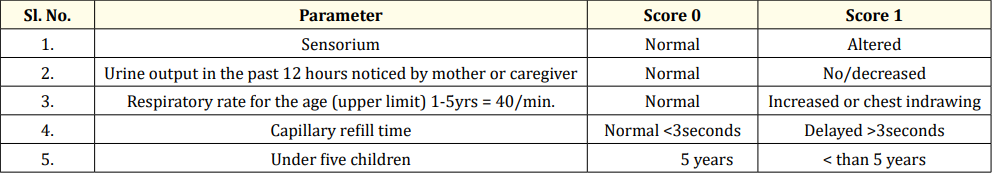
Table 1: SURCU5 scoring system for sick children between 1 to 5 years of age.
This simple practical clinical risk tool taught and explained in local Telugu language to nursing staff. They were trained to calculate the scores of sick children and bypass the long awaiting out patient queue if children score 3 or more. These very sick children directly brought to physician consultation for examination, hospitalisation for inpatient care or prompt referral to a medical college hospital. This risk score based care model resulted in prompt attention and management of those under 5s with disease severity. This clinical practice resulted in almost zero mortality at our health care facility.We were practicing this tool for a decade and more.
Predictive scores for estimating disease severity and ongoing clinical deterioration like PEWS scores [14] already in use. These scores had scoring of 0 to 3 with 4 parameters for calculating which is quite difficult for nurses and residents to remember. This needs documentation by scoring on offline or online charts. A prediction score with few parameters - five or less and scoring of 0 to 1 is easy to remember and practice by both medical and paramedical health personnel especially at resource limited settings. Our “SURCU5” prediction score probably answers this question in estimating disease severity at presentation, further clinical deterioration or improvement upon hospitalization by repeating the score and in decision taking whether to continue management or referral to higher care facility.
Simple Clinical risk score tools help healthcare professionals to
Various clinical risk scores are available for clinical practice. These scores are essential but complex and in use for diagnosing and grading the disease severity.
Simple and practical clinical risk score with less parameters and scoring for paediatric purpose is needed for daily practice (for busy clinics and hospitals in tropical countries during seasonal surge of endemic diseases). SURCU5 clinical score is a simple and practical, conceptualized research work intended for better utilisation of limited resources (at small scale healthcare facilities with men 10 -50) during surge of endemic diseases.
This is a conceptualized research work in a single health care facility, and we were not published the data regarding the same. This needs to be practiced and evaluated in other health care centres for care optimization and before recommendation.
There are no conflicts of interest for this work.
Copyright: © 2023 Chakradhar Maddela. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.