Aktas Selma1* and Nur Seyma Zengin2
1 Acibadem University Medical Faculty, Department of Pediatrics, Division of
Neonatology, Turkey
2
Gaziosmanpasa Taksim Research and Training Hospital, Turkey
*Corresponding Author: Selma Aktas, Acibadem University Medical Faculty, Department of Pediatrics, Division of Neonatology, Turkey.
Received: November 16, 2020; Published: December 10, 2020
Citation: Aktas Selma and Nur Seyma Zengin. “An Unexpected Outcome of Congenital Intrahepatic Arterioportal Fistula with Trisomy 21”. Acta Scientific Paediatrics 4.1 (2021): 06-08.
Congenital intrahepatic arterioportal fistula is a rare condition and presents with symptoms of portal hypertension. Congenital cardiac anomalies are common among children with Trisomy 21 and there is also an association between Trisomy 21 and congenital vascular malformations of the liver. We discuss a patient with Trisomy 21 that presented with continuous murmur in the right upper quadrant of abdomen, thrombocytopenia and mild pulmoner hypertension and diagnosed as congenital intrahepatic arterioportal fistula by doppler USG and angiography. Surprisingly the shunt regressed spontaneously without any intervention.
Keywords: Trisomy 21; Congenital İntrahepatic Arterioportal Fistula
Congenital Intrahepatic Arterioportal Fistula (IAPF) can be defined as an intrahepatic communication between the hepatic artery and the portal venous system without secondary cause or primary hepatic or biliary disease [1]. Although congenital cardiac diseases are very common in Trisomy 21, congenital vascular malformations (CVMs) of the liver are so rare and there are some case reports published in the literature [2]. IAPFs in infant usually present with gastrointestinal bleeding, ascites, splenomegaly, failure to thrive, diarrhea and malabsorption [1]. Treatment options are surgical, percutaneous transarterial embolization (TAE) and a combination of TAE and surgery [2].
We want to share a case of congenital IAPF associated with Trisomy 21, suspected on the 4th day of life and diagnosed in the first week of life. To our knowledge he is the youngest patient in the literature diagnosed as IAPF association with Trisomy 21.
A 1940 g male infant was born at 37 weeks of gestational age by cesarean section to a 36 year-old mother owing to fetal distress. The APGAR scores were 7 and 9 at 1st and 5th minutes, respectively. The newborn was transferred to neonatal intensive care unit (NICU) due to respiratory distress. He was supported by nasal continuous air-way pressure (N-CPAP). He had the phenotypic features of Trisomy 21 including flat nasal bridge, protruding tongue, epicanthal folds and karyotypic evaluation confirmed trisomy of chromosome 21. On physical examination we heard grade 3/6 murmur and Echocardiography demonstrated ventricular septal defect (VSD), secundum atrial septal defect (ASD) and mild pulmonary hypertension. He had thrombocytopenia on the first day of life and following days (91000- 85000- 27000- 144000- 115000 /uL). He was transfused once when the level was 27000/uL. The thromboctye level was normal on 9th day of life and thereafter. Antibiotherapy was started for early neonatal sepsis suspicion. On the 4th day of life auscultation of a continuous murmur was noticed in the right upper quadrant of abdomen, for hepatic USG and doppler USG was evaluated. The common hepatic artery originated from abdominal aorta was dilated and interconnection between left hepatic artery and horizontal segment of left portal vein was demonstrated in the liver and evaluated as congenital IAPF by Doppler USG (Figure 1, 2 and Figure 3) Please add the figures after the references. Hepatic veins were wide in caliber that indicated right heart insufficiency; so captopril and loop diuretics were started. The diagnosis was confirmed by angiography (Figure 4). The baby was so little and not so symptomatic; For repetition of angiography 4 to 6 months later was planned according to the concensus of neonatologist, pediatric cardiologist, cardiovascular surgeon and interventional radiologist. He was discharged with captopril and loop diuretic treatment. The angiography was repeated 4 months later to evaluate IAPF and to perform angiographic intervention with coil embolization for closure the shunt but IAPF was not demonstrated, the interconnection between left hepatic artery and horizontal segment of left portal vein regressed spontaneously.
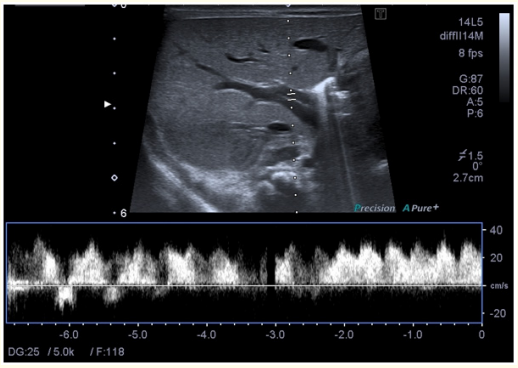
Figure 1
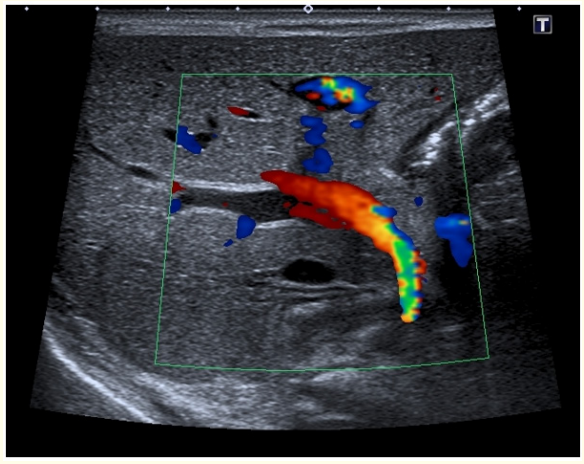
Figure 2
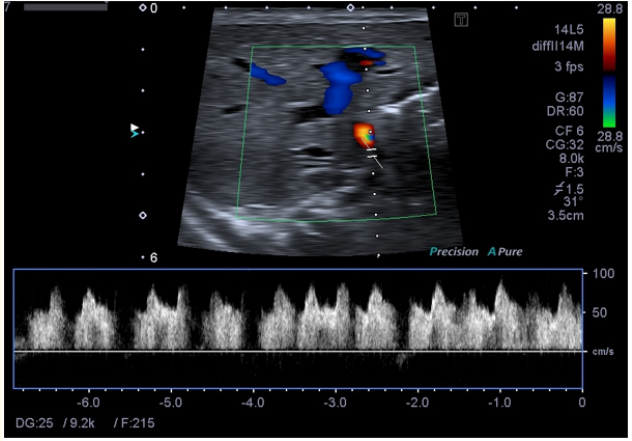
Figure 3
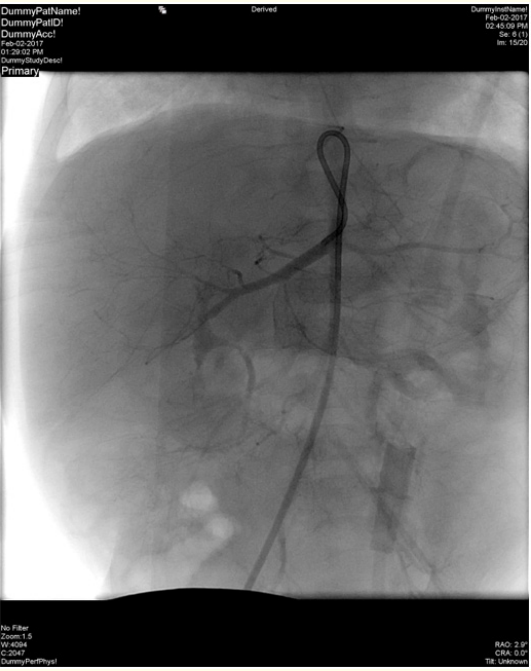
Figure 4
Congenital cardiac anomalies [3], and intra-abdominal malformations such as duodenal atresia [3] are common in children with trisomy 21; besides these associations in recent years some studies demonstrate a relation between trisomy 21 and CVMs of the liver [3]. CVMs of the liver can be defined by the degree of interconnection between the hepatic arterial and portal venous network and systemic venous drainage [3]. Congenital intrahepatic arterioportal fistula (IAPF) which is one of the CVMs of the liver, is a rare condition in children. Most of them are secondary to trauma, iatrogenic injury (such as liver biopsy), tumors and aneurysms [4]. Only %15 of IAPFs are congenital [4] and present early in infancy with signs of heart failure, portal hypertension (splenomegaly, esophageal varices, recurrent gastrointestinal bleeding, ascites, malabsorption and abdominal pain), poor feeding /failure to thrive, thrombocytopenia, coagulopathy, auscultation of a continous murmur in the right upper quadrant and jaundice [3]. The variable presentation of congenital IAPF is related to the variations in fistula location and shunt size [5]. Children are usually more resistant to hepatic encephalopathy than adults [2]. Present case was so young and shunt size was not so wide, for the signs of portal hypertension were not noticed. The main sign that cause us to suspect IAPF was auscultation of a continous murmur in the right upper quadrant and the others are thrombocytopenia and mild heart failure. The liver and renal function tests were all normal. There was no history of trauma, surgery or catheterization so the IAPF was determined as congenital.
There are different classifications in the literature; ‘NortonJacobson’ classification of IAPF according to the afferent vessels supplying them is unilateral, bilateral or complex. An unilateral IAPF (Type 1) is supplied by only one of the right, left or main hepatic artery. A bilateral IAPF (Type 2) is supplied by both left and right hepatic arteries or their branches. Complex lesions (Type 3) consist of a plexiform vascular nidus with multiple feeding arteries [5]. According to ‘Norton-Jacobson’ classification, IAPF of present case was type 1; there was interconnection only between left hepatic artery and left portal vein. Burdall., et al. [3] determined the CVMs of the liver as Group (i) and Group (ii). Group (i) is connection between the portal venous and systemic venous systems; Group (ii) is connection between hepatic arterial and either or both portal venous and systemis venous systems. Congenital connection between the arterial and venous system is the least common CVM in the literature. According to second classification our case was included in Group (ii).
Although a solitary fistula is usually acquired, diffuse or multiple IAPFs are almost all congenital. Less than 10% of all arterioportal fistulae that involve the hepatic artery are congenital [5]. Present case had a congenital IAPF but contrary to expectations it was solitary, not diffuse or multiple.
Ultrasonography is the first line imaging modality in IAFP [5]. Hepatic angiography confirms the diagnosis and demonstrate the vascular anatomy. There is not usually a structural anomaly of the liver on computed tomograhy or magnetic resonans imaging [4]. Treatment options are surgical, TAE and a combination of TAE and surgery. Any of the options is selected according to the fistula location, lesion extent, accurate localization of all shunts and hospital experience. TAE is safer, cheaper and more practical. The other advantages are shorter hospital stay, decreased pain and repeated acces availability. TAE is very likely to be effective for unilateral lesions [5]. Complex congenital IAPF are prone to colleteraliztion or recurrence after TAE [5]. So complex congenital IAPF may necessitate to treat with a combination of surgery and TAE (5). In the present case IAPF was diagnosed by dopplerr USG and angiography was performed to demonstrate the anatomy of the fistulae correctly. No treatment was made during the first angiography because the infant was so little and not so symptomatic. Repetition of angiography 4 to 6 months later was planned for performing TAE. Surprisingly the interconnection between left hepatic artery and horizontal segment of left portal vein had regressed spontaneously so IAFP was not demonstrated on the repeated angiography 4 months after the first evaluation.
Burdall., et al. report CVMs of the liver associated with Trisomy 21 in company with English language literature. They present 4 trisomy 21 patients who have arteriovenous CVM of the liver, and none of them regressed spontaneously [3].
In conclusion literature shows an association between congenital cardiac and hepatic vascular malformations in infants with Trisomy 21, so infants with Trisomy 21 should be followed for the signs of congenital CVMs of the liver in addition to congenital heart defects.
All the authors report no conflicts of interest.
Parents gave their permission to publish the case report.
Copyright: © 2021 Aktas Selma and Nur Seyma Zengin. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.