Jarupat Jundaeng1*, Rapeeporn Chamchong2 and Choosak Nithikathkul3
1Dental Department, Fang Hospital, Chiangmai Province, Tropical Health Innovation Research Unit, Faculty of Medicine, Mahasarakham University, Thailand
2Department of Computer Science, Faculty of Informatics, Mahasarakham University, Thailand
3Tropical Health Innovation Research Unit, Faculty of Medicine, Mahasarakham University, Thailand
*Corresponding Author: Jarupat Jundaeng, Dental Department, Fang Hospital, Chiangmai Province, Tropical Health Innovation Research Unit, Faculty of Medicine, Mahasarakham University, Thailand.
Received: August 08, 2024; Published: August 29, 2024
Citation: Jarupat Jundaeng., et al. “Esthetic Management of Altered Passive Eruption: A Clinical Case Report". Acta Scientific Dental Sciences 8.9 (2024):92-98.
Aim and Background: This report outlines the diagnosis, treatment, and follow-up of a 30-year-old female patient with altered passive eruption (APE) leading to a pronounced gummy smile. The condition was managed using gingivectomy and osseous surgery to achieve esthetically and functionally favorable results. Case Description: The patient, who presented with short clinical crowns and excessive gingival display, was diagnosed with APE Type IB, characterized by a thick, flat gingival phenotype and a gingival margin positioned 3-4 mm above the CEJ. The treatment involved apically repositioning the gingival margin through gingivectomy and osseous surgery to increase clinical crown length and improve smile aesthetics. The procedure was performed under local anesthesia.
Results: Follow-up at 7 days and 3 months showed complete soft tissue healing, with the patient expressing high satisfaction with her improved smile. Minimal postoperative discomfort was reported, underscoring the efficacy of this approach in managing APE.
Conclusion: Gingivectomy combined with osseous surgery effectively treats APE, significantly enhancing dental esthetics and patient confidence. This case underscores the importance of accurate diagnosis and personalized surgical strategies for optimal esthetic outcomes.
Clinical Significance: This case highlights the importance of tailored surgical interventions in enhancing dental aesthetics and patient satisfaction in APE management.
Keywords: Altered Passive Eruption; Crown Lengthening; Gingivectomy; Esthetic Dentistry; Gummy Smile
A beautiful smile plays a crucial role in enhancing facial aesthetics, significantly boosting an individual’s charm, confidence, and perceived friendliness. The aesthetics of a smile are influenced by several factors, including facial symmetry, the alignment of the smile line, the contour and health of the gingiva, as well as the shape, size, and positioning of the teeth [1]. One of the challenges in maintaining a pleasing smile is managing excessive gingival display, commonly referred to as a "gummy smile," where more than 2 millimeters of gingiva are visible when smiling [2]. This condition can negatively impact the overall aesthetic appeal of the smile, leading to self-consciousness and dissatisfaction in affected individuals [3].
Esthetic crown lengthening is a well-established surgical procedure designed to enhance the appearance of the teeth and smile by addressing issues related to excessive gingival display [4]. The procedure involves reshaping the gingival tissues and, in some cases, the underlying bone to expose more of the tooth's surface [5]. This not only improves the tooth-to-gum ratio but also creates a more balanced and harmonious smile [6]. Crown lengthening is particularly beneficial for patients with altered passive eruption (APE), a condition where the gingiva fails to recede adequately after tooth eruption, resulting in a shortened clinical crown [7].
Altered passive eruption is a significant contributor to gummy smiles, affecting approximately 10.57% of the population, with a higher prevalence among females, particularly those aged 20-30 years [8]. APE is characterized by an incomplete apical migration of the gingival margin during tooth eruption, which leads to excessive gingival coverage of the tooth [9]. This condition not only compromises the esthetic proportions of the teeth but also complicates oral hygiene, potentially leading to periodontal issues [10].
This case report focuses on the diagnosis and esthetic management of a patient with altered passive eruption using crown lengthening techniques. The aim is to highlight the effectiveness of this approach in restoring a balanced smile and enhancing the patient's overall facial aesthetics [11]. By addressing the specific needs of patients with APE, esthetic crown lengthening offers a targeted solution that can significantly improve both the function and appearance of the teeth, leading to higher patient satisfaction and confidence [12].
A 30-year-old Thai female, single and employed as a government officer, patient presented to the periodontist with the primary complaint of short teeth and excessive gingival display when smiling (Figure 1). She reported that this condition had been present for several years. The patient had no known serious illnesses or drug allergies, and her vital signs were within normal limits (BP 121/87 mmHg, PR 82 bpm). Her dental history included regular annual check-ups and scaling.

Figure 1: The patient’s primary complaint of short teeth and excessive gingival display when smiling.
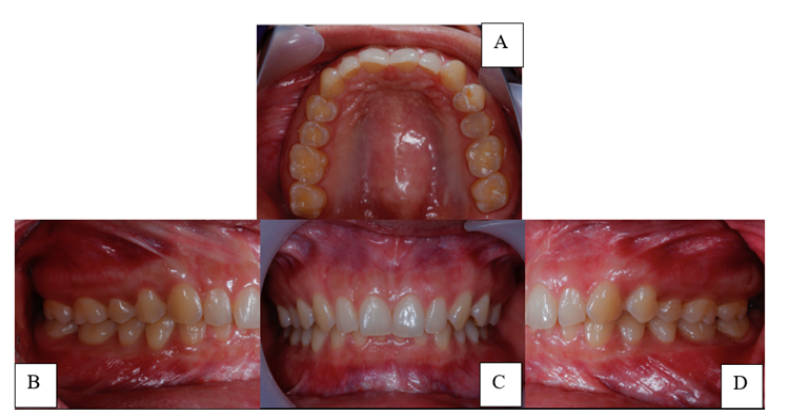
Figure 2: Intraoral examination before treatment: A shows the occlusal view, B shows the right buccal view, C shows the frontal view, and D shows the left buccal view
The periapical radiographs reveal that the alveolar bone crest is close to the cementoenamel junction (CEJ), indicating minimal bone recession and a coronal position of the gingival margin prior to surgery, which required osseous surgery for effective crown lengthening. Additionally, there is no evidence of periapical pathology, such as radiolucencies or granulomas, confirming that the teeth are free from endodontic issues and are suitable candidates for esthetic crown lengthening (Figure 3).
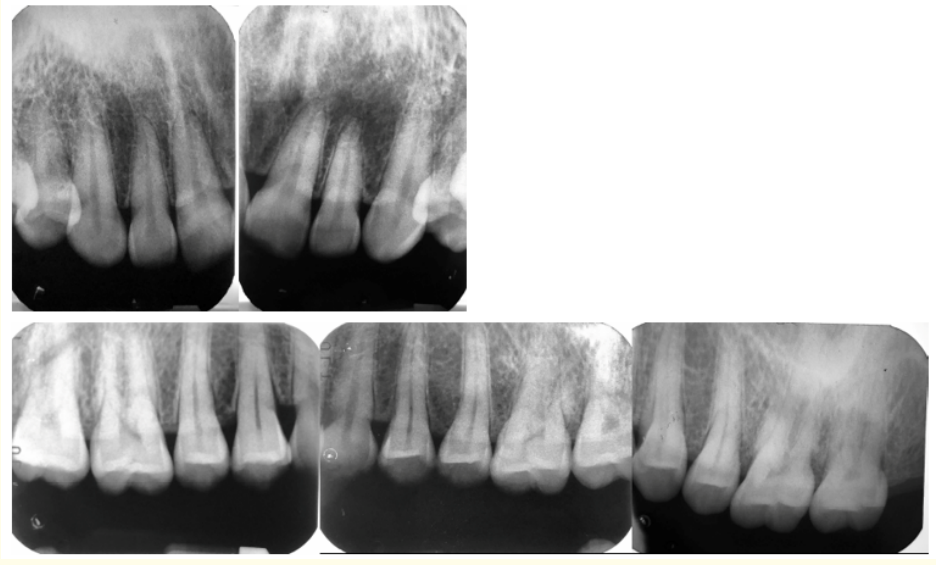
Figure 3: Radiographic examination: Periapical radiographs of the upper teeth.
Altered passive eruption Type IB [7], characterized by an adequate amount of keratinized gingiva and the osseous crest at or near the CEJ.
The treatment involved gingivectomy combined with osseous surgery to reposition the gingival margin apically and lengthen the clinical crown. An apically positioned flap was created, and osteoplasty and ostectomy were performed to achieve the desired outcome.
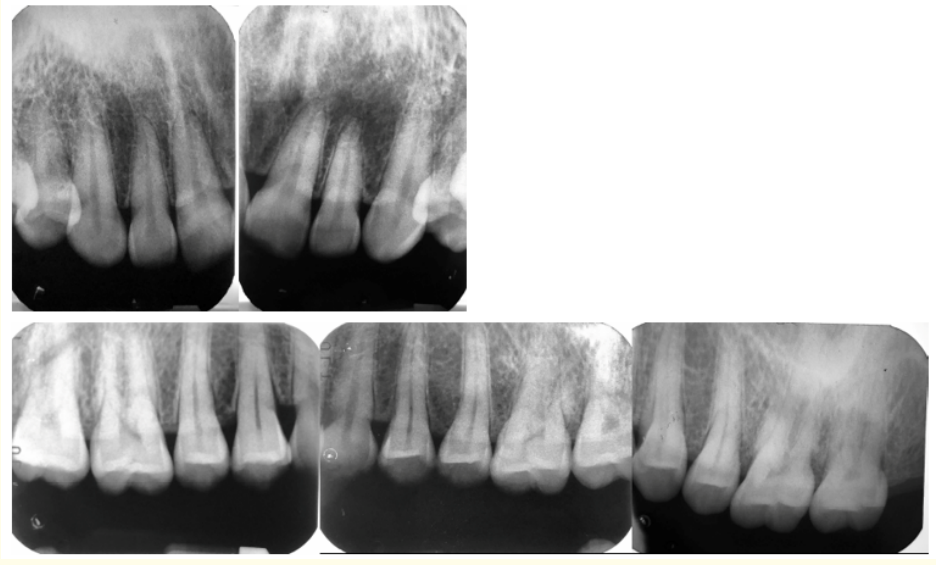
Figure 4: Incision line design for gingivectomy from tooth no. 16 to 26
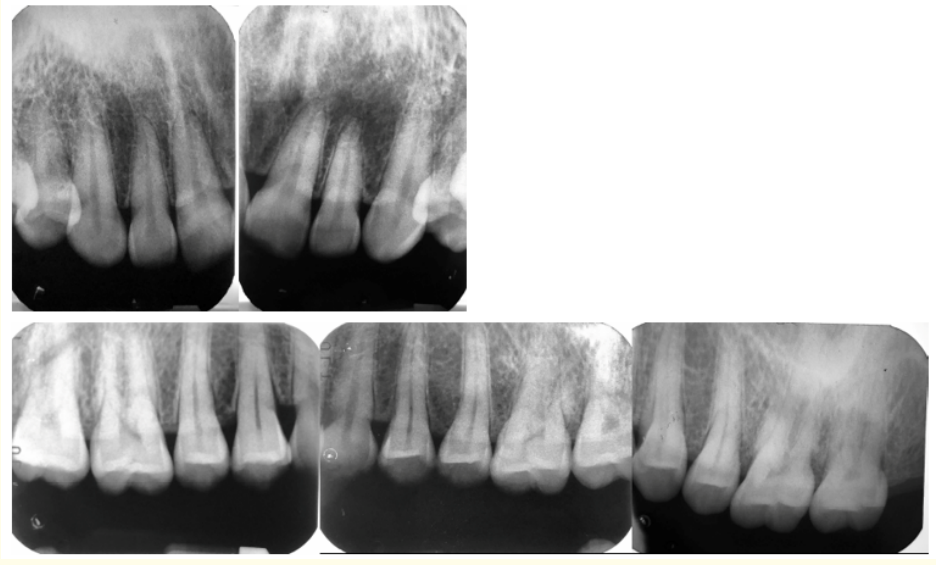
Figure 5: Treatment Procedure: A shows blade no. 15C, B shows the incision line, C shows the reflected flap revealing bony exostosis, D shows the result after ostectomy and osteoplasty to achieve a positive architecture, E shows a continuous sling suture, and F shows complete healing.
The patient underwent esthetic crown lengthening surgery with the following steps: Local infiltration anesthesia was administered using 4% articaine with 1:100,000 epinephrine. A total of 5.1 mL was injected around teeth 16-26. The gingival margins for teeth 16-26 were symmetrically marked. An internal bevel incision was made 2-3 mm from the original gingival margin, sparing the interdental papillae. Sulcular incisions extended to the mesiobuccal line angles of teeth 16 and 26, followed by vertical releasing incisions to the mucogingival junction. A full-thickness flap was raised, exposing the entire alveolar bone. Inflammatory tissue was removed, and root planning was performed. Osteoplasty and ostectomy were conducted to contour the bone, ensuring a 2 mm distance between the alveolar crest and the CEJ. The flap was repositioned 1 mm coronal to the CEJ, and sutured using 4-0 Vicryl with a continuous sling suture technique (12 stitches). A periodontal dressing was applied. Postoperative pain was managed with 400 mg ibuprofen as needed, and infection was prevented with a 7-day course of 500 mg amoxicillin. The patient was advised to apply cold compresses, avoid brushing the surgical area, and use 0.12% chlorhexidine mouthwash twice daily. Suture removal was scheduled for one week later.
During the first follow-up at one week (Figure 6), the patient reported mild discomfort during the first two days post-surgery but was otherwise asymptomatic. Upon suture removal, the gingiva appeared slightly inflamed but with no signs of infection. The gingival margins remained stable. At the three-month follow-up (Figure 7), the gingiva showed excellent healing, with tight adaptation around the tooth necks and fully regenerated interdental papillae. Slight plaque accumulation was noted, and the patient was reminded of proper oral hygiene practices. The patient expressed high satisfaction with the esthetic outcome, noting a significant reduction in gingival display and increased confidence while smiling. The clinical crown height increased by an average of 2.4 mm, with minimal soft tissue rebound (0.2 mm) and more than 3 mm of keratinized gingiva remaining.

Figure 6: Clinical Outcomes at 1-Week Follow-Up: A shows the frontal view before treatment, B shows the smile line before treatment, C shows the frontal view after treatment, and D shows the smile line after treatment.
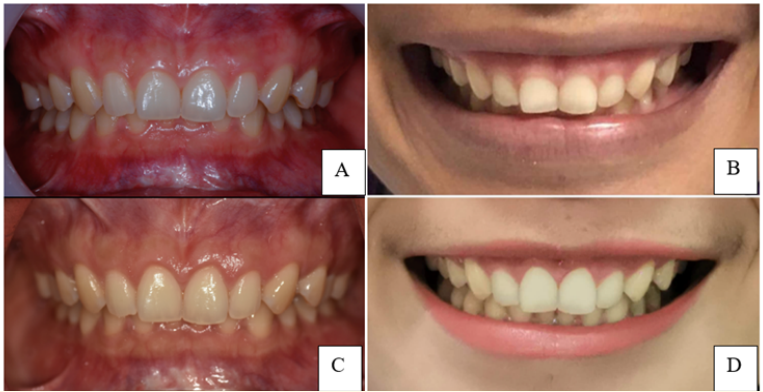
Figure 7: Clinical Outcome at 3-Month Follow-Up: A shows the frontal view before treatment, B shows the smile line before treatment, C shows the frontal view after treatment, and D shows the smile line after treatment.
This case report highlights the successful management of altered passive eruption (APE) Type IB in a 30-year-old female patient presenting with a chief complaint of short teeth and excessive gingival display. The patient exhibited a thick, flat gingival phenotype, with a gingival margin positioned 3-4 mm above the cementoenamel junction (CEJ) and probing depths ranging from 1-3 mm without gingival recession [7,9]. The clinical findings and diagnosis align with the characteristics of APE Type IB, as classified by Coslet et al., where there is an adequate amount of keratinized gingiva and the osseous crest is at or near the CEJ [7]. The treatment plan involved a gingivectomy combined with osseous surgery, which is the recommended approach for managing APE Type IB to achieve a more esthetically pleasing smile by repositioning the gingival margin apically and increasing the clinical crown length [4]. This method not only addresses the excessive gingival display but also improves the tooth-to-gingiva ratio, which is crucial for esthetic outcomes [12].
Postoperative healing was uneventful, with the patient experiencing only mild discomfort that required analgesics for 1-2 days, consistent with findings from previous studies on esthetic crown lengthening [13,14]. By 3-month, complete soft tissue healing was observed, and the patient reported high satisfaction with the esthetic outcome, which is in line with other studies that emphasize the importance of patient satisfaction in the success of esthetic dental procedures [8,11].
Moreover, the minor reduction in crown height at the three-month follow-up compared to the immediate postoperative measurement is consistent with the expected soft tissue rebound following crown lengthening procedures [15,16]. This outcome underscores the importance of precise pre-surgical planning, including bone reduction to accommodate the biologic width, which averages 2.04 mm [17]. Failure to account for this dimension can lead to complications, such as inadequate gingival contour or periodontal issues post-surgery [18].
The successful management of altered passive eruption through gingivectomy and osseous surgery highlights the importance of tailored treatment approaches in esthetic dentistry. The patient’s case demonstrates that accurate diagnosis and appropriate surgical techniques can lead to significant esthetic improvements and increased patient satisfaction.
This case report provides evidence for the effectiveness of crown lengthening procedures in treating altered passive eruption, contributing to the enhancement of dental esthetics and patient confidence.
This study, while successful in managing altered passive eruption with esthetic crown lengthening, has several limitations. First, the follow-up period was limited to three months, which may not fully capture long-term outcomes such as soft tissue stability and patient satisfaction. Longer follow-up intervals of six months to a year are recommended to observe potential soft tissue rebound and ensure sustained esthetic results [15]. Additionally, the study was conducted on a single patient, which limits the generalizability of the findings. A larger cohort study would be beneficial to validate the effectiveness and predictability of this treatment approach across a broader population [16].
Future studies should focus on long-term evaluations of esthetic crown lengthening in patients with APE, assessing both clinical and patient-reported outcomes over time. Comparative studies involving different surgical techniques or adjunctive therapies, such as the use of laser or piezosurgery, could provide insights into optimizing treatment protocols for various gingival phenotypes. Moreover, investigating the role of preoperative digital smile design and 3D imaging could enhance treatment planning and predictability, ultimately leading to better patient outcomes [17,18].
Copyright: © 2024 Jarupat Jundaeng., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.