Bibiana Fabado Martínez, Melanie Lozano Pajares, Otto Alemán Miranda*, Mª Celia Haya Fernández, Alina Rodríguez Castellanos
General Clinical and Surgical Hospital, Orlando Pantoja Tamayo, Cuba
*Corresponding Author: Otto Alemán Miranda, General Clinical and Surgical Hospital, Orlando Pantoja Tamayo, Cuba.
Received: July 24, 2024; Published: August 21, 2024
Citation: Otto Alemán Miranda., et al. “Risks in Patients with Prosthetic Treatments". Acta Scientific Dental Sciences 8.9 (2024):44-57.
Prosthetic treatments are variable in duration and complexity of the case to be rehabilitated. An adequate selection of the procedure for each patient that is evaluated independently is essential. Most consultations are scheduled, with predictable clinical results and there are usually few emergencies. Therefore, a bibliographic review was carried out with the objective of showing the main risks and complications of prosthetic rehabilitation treatments.
Keywords: Risk; Dental Prosthesis; Fixed; Removable
The success and quality of treatments is only achieved when professionals control the possible risks and the margin of error present both in the clinic (with the patient) and in the laboratory (with the working models), in addition, the actions Coordinated procedures ensure the longevity of the prostheses and the proper management of the patient, who expects the dentist to fully satisfy their functional and aesthetic needs; In the same way that the dentist expects the dental technician to satisfy his expectations by providing prosthetic work in which he does not have to make major corrections or wear, that is, quality work.
Risks in the clinical and laboratory steps for making a dental prosthesis.
Repetitions of laboratory work on dental prosthesis increase the number of appointments used by patients depending on the type of treatment in oral rehabilitation, marking significant differences between the ideal and actual stay of these treatments. The same happens with the repetitions of diagnostic and definitive impressions and other clinical steps, which shows a greater expenditure of resources and time used for patient treatment, affecting patient satisfaction. In the same sense, many professionals do not take sufficient care when planning, operating and guiding the production laboratory, the work of removable partial dentures and fixed partial dentures.
They report that many of the failures and repetitions occur due to inadequate communication between the dentist and the laboratory technician responsible for the work, to whom a large part of the responsibility is delegated, especially with regard to fixed prosthesis work, which receives insufficient information, poor impressions and inadequate records. Production orders are explanatory, indicative of the work to be carried out by the technician who receives the model, whether work or study, and there is a tendency to downplay its importance [1,2].
They are not always accompanied by the corresponding notes with the modifications, care, clarifications relevant to the patient's anatomical or functional clinical problems that are not observed in the inert model, but that are visualized in the clinic or are sometimes not read by the staff, from the laboratory, and, therefore, they are not met, sometimes leading to failure or dissatisfaction not only of the operator, but also of the patient who is going to receive the prosthesis. Repetitions of dental laboratory work affect the efficiency of the dental service, due to the duplication of expenses, including additional materials and not only the dissatisfaction with the time used for the treatment, but also the impact on patient care by the work team constituting unwanted abuse [1,3].
During rehabilitative treatments for the construction of any type of prosthesis, a detailed clinical history (anamnesis, clinical examination and complementary examinations) is first carried out, which leads to the establishment of the diagnosis, prognosis and treatment plan. If a complete and thorough examination of the patient's oral conditions is not carried out, it is impossible to correctly identify the present problem and plan the appropriate treatment to restore lost functions, as well as guarantee the greatest possible comfort and aesthetics. A careful and detailed anamnesis is essential in the clinical method, as well as knowing the systemic diseases that may have influenced the state of oral health, and if necessary, referring to the indicated specialist.
The clinical examination must thoroughly cover every region of interest to discover any signs present and recognize the characteristics of the elements of the paraprosthetic organ, through inspection, palpation, percussion and auscultation. Complementary examinations are useful to corroborate the diagnosis and provide elements to establish the prosthetic treatment plan. Not following these rules decreases the chances of success in treatments. The importance of the clinical history is fully justified from the healthcare, ethical and medico-legal point of view and must comply with the veracity, accuracy and technical rigor of the records. 1.1. Risks in taking initial records. Primary impressions are made, in most cases, with alginate, although other materials such as silicones or polysulfides are also valid, from which the study models are made for the preparation of individual trays [1-4].
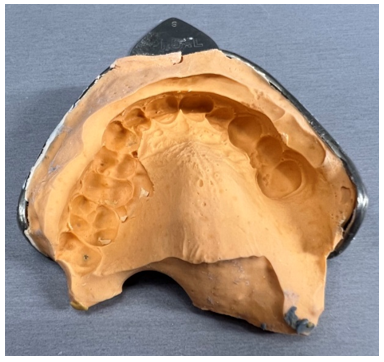
Figure 1: Low quality preliminary impression, note the impression defects at the level of the premolars.

Figure 2: Final impression taken without references of the remaining teeth in the mouth.
This makes the job of the laboratory technician difficult. Downplaying its importance, as frequently happens, ignoring this clinical step, and directly taking the final impression, without properly individualizing the tray, constitutes an attack on the tissues directly related to the prosthetic device, increasing the risk of adaptation problems.
The success of a print depends on several factors, including:
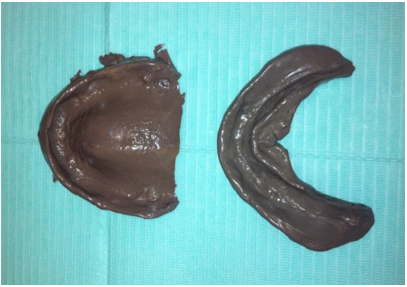
Figure 3: Final impressions with polysulfide taken with individual trays for a removable total prosthesis.
Furthermore, there are various potential sources of error including distortion of impression materials, disinfection process, transportation of impression tray to dental laboratory under different weather conditions.
Errors in this conventional workflow can become responsible for the lack of final adaptation of the restoration and its subsequent loss. Studies obtain results in the precision of the marginal adjustment above 165 μm, considering the preparation of the dental crown, exceeding the clinically acceptable limit (100 μm). The most complex step in the process of making a dental prosthesis is achieving an accurate impression of the carved or uncut teeth, dental implants, or any intraoral defects. The professional must achieve an exact duplication of the anatomy, so that the laboratory technician can create the restoration that is an exact replica of the destination site [4-6].
In recent times, digital work offers advantages both in the consultation, laboratory and patient comfort. Three-dimensional scanning of the mouth is used in a large number of procedures in dentistry, such as restorative, surgery and orthodontics. The first step of all digital work is the optical intraoral impression. Which allows you to immediately check the quality of the impression, including the geometry of the abutment and the finishing line of the prepared tooth. If the professional is not satisfied with the scan, it can be repeated at the same appointment. This is why this technique contributes to more efficient work in the dental office. The use of impressions in trays and their consequent material is avoided and this contributes to the patient's well-being [1,2,7].
When talking about the use of computer-aided technologies for the production of dental restorations, the minimum requirements are to digitize the tooth or teeth to be restored. Precision in digitization is a primary factor that influences the survival of restorations. Currently, digitization can be performed directly in the patient's mouth (intraoral) or indirectly after taking the impression and manufacturing the model (extraoral).
Taking definitive records with individual buckets.
To avoid failures, it is necessary to clarify in the production order sent to the laboratory what type of cuvette is needed for each case. Spaced and perforated individual tray for alginate, spaced and smooth individual tray for plaster, or fitted and smooth individual tray for light silicone and zinquenolic paste, if the perforation of the tray in the area corresponding to the palate is insufficient to expel Excess material and trapped air can alter the registration of details at this level.
The risks of failure during this clinical step are not putting it in the mouth in a plastic state, so it would not preserve the shape and extension of the surface to be reproduced. Not completely covering the surface that the prosthesis should cover reduces the support surface and, therefore, the retention and stability of the prosthesis [5-8].
The definitive compressive impression produces gradual bone resorption by keeping the tissues under constant pressure. These must be mucostatic, passive or with minimal pressure. From this final impression, the working models are obtained from which the base plates with the articulation wheels can be obtained. Taking intermaxillary records with base plates and articulation rims.
A well-made base plate facilitates the taking of intermaxillary records, which can be diagnostic or as a clinical procedure required for the preparation of the stomatological prosthesis. According to the experience of numerous specialists, it is a difficult clinical step and of great importance for successful rehabilitation of aesthetic, mechanical and functional aspects such as chewing and phonation, in correspondence with the individual characteristics of the totally and partially edentulous patient, determining the vertical dimension. and mandibular centric relation. The bases used to obtain the records must have certain characteristics such as

Figure 4: Final working model of poor quality, see the defect at the level of the carved pillar.
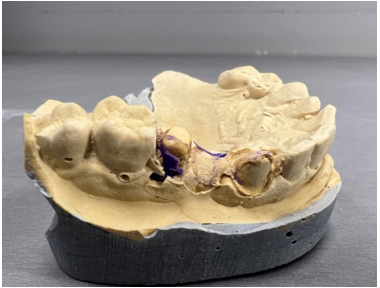
Figure 5: Final working model with defects in the carved pillars.
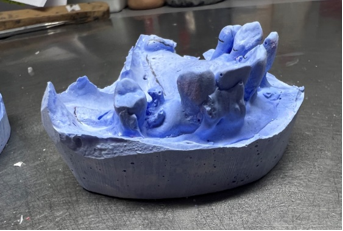
Figure 6: Poor quality working model.
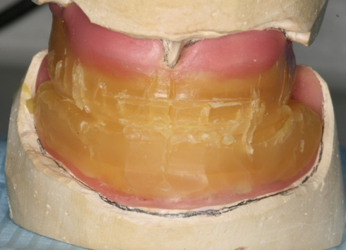
Figure 7: Base plates with rims and intermaxillary relationships.
In addition, they have several purposes, since they allow: a) transport the occlusion rollers for the registration of craniomandibular relationships. b) place the teeth in the wax-up test. c) review the accuracy of the previously taken intermaxillary records.
This step can fail both due to technical factors in the laboratory, as well as those inherent to the patient or the operator.
The most frequent errors in the craniomandibular relationship may be related to the material used in the articulation plates, if they are not well adapted, short or overextended, with the technique: poor positioning or fatigue of the patient, incorrectly interpreted order, uneven softening of the labrum, expulsive dental occlusion, painful or depressible supporting tissues, gag reflexes, lip deformations, mandibular deviations or other pathological causes [10].
Among other
Clinical manifestations in changes in vertical dimension. The alteration of the vertical dimension has been a controversial aspect for more than 50 years, since today there is no exact protocol to determine this measurement in a precise way for each person, but there are several proposals described by various authors that help the professional to carry out treatments that do not cause any type of joint, muscular, functional or aesthetic alteration [12-14].
The patient's Vertical Dimension in Occlusion (VOD) is usually determined by the teeth present in the mouth that are in maximum intercuspation. When they are lost, among the consequences of edentulism is the loss of vertical dimension, which can alter the chewing function, phonetics, dental aesthetics and facial appearance, and this is when we speak of an alteration of the vertical dimension. Restoration of the OVD achieves balance and harmony of the lower third of the face and ensures the most ideal function.

Figure 8: Edentulous patient with loss of vertical dimension.
Therefore, any oral rehabilitation treatment needs to restore the physiological vertical dimension by replacing the lost teeth and associated tissues. Regarding the decreased vertical dimension, it does not produce tension as it does not reduce the length of the muscles, clinically it is characterized by the reduction of the lower facial third, decreased thickness of the lips, mandibular prognathism, angular cheilitis, interposition of the tongue between the occlusal surfaces of the teeth and possible pathology of the temporomandibular joint.
Regarding the increased vertical dimension, it is characterized by high visibility of the teeth, incompetent lip closure, headache in relation to muscle function and subjective sensation of a foreign body inside the mouth; The body tries to adapt with intrusion of the teeth into the alveolar bone or bruxism. The increase in dental load due to the muscles' attempt to recover their normal length, if it exceeds the adaptive capacity of the supporting tissues, would cause hypermobility and decreased periodontal resistance, alveolar atrophy, dental fractures, occlusal disharmonies, invasion of free space with phonic alterations, sucking and whistling actions, and muscle dysfunction [1,2].
The most frequent errors that expose the result of the vertical dimension registration to failure are the following: - Error in the assembly of the models in the articulator. - Errors during the assembly of teeth by the dental laboratory. - Lack of communication between the dentist and the laboratory technician. 1.5. Risks in the selection, assembly and testing of artificial teeth. When selecting artificial teeth, the professional must apply his artistic mastery, especially when there is variation in the color of the remaining teeth caused by old fillings, color changes due to blows or root treatments, as well as alterations in the shape and color of the teeth. remaining teeth [1,2].
It is important that there is close collaboration between the laboratory technician and the dentist, and not to underestimate the opinions of the patient and his environment, essential for the selection of the shape, color and size of the teeth, determinants in the facial expression that provide to. Large differences between the teeth of both arches or intraarch would be unsightly. It is a common error not to select the color in natural light, and another quite common error is not to moisten the teeth from the shade guide, or to dry the teeth in the patient's mouth looking for similarity in the refraction and reflection of the light received, as well as such as within the operator's field of vision, strong colors that can generate complementary colors, which are even related to the painting of the walls of the dental clinic [13-15].
The assembly of artificial teeth is a laboratory procedure, but the clinician must know it to be able to make the pertinent corrections and indications and exchange the details of the case with the technician. When mounting the models in the articulator, special attention must be paid to carry out this procedure very accurately and not modify the relationships obtained. In the tooth test, if the models are not received in the articulator with the laboratory note and the instructions made by the prosthodontist to the dental technician, important details to be checked may be lost, such as the correct mounting of the models in the articulator, the vertical dimension, adaptation and conformation of the bases, correct assembly of the teeth, the occlusal plane, waxing of the models, adequate occlusion and articulation, lower teeth centered on the ridge, as well as the correct cusp-fossa relationship.
In the mouth, the aspects related to this step cannot be ignored, such as checking retention, support, stability, aesthetics, phonetics, occlusion and comfort, so it is recommended to do it in an orderly manner, otherwise there is a risk of omitting it. any of these requirements.

Figure 9: Teeth test and verification of all the mentioned parameters and taking eccentric records to balance the total prosthesis.
If there is no correct release of the frenulums, extension and adaptation of the bases, the biomechanical principles and phonetic tests cannot be verified. Forced laughter in patients can falsify the verification of the correct height of the teeth. The patient must be made to smile in a persuasive way. If the patient cannot bite the lower lip, it is advisable to repeat the lower lip, otherwise the liquids will be spilled in addition to being unsightly. Any error observed in centric occlusion requires obtaining a new measurement of the craniomandibular relationship to avoid treatment failure [1,2,15-17].
A very thick palatal vault, very short teeth, lack of peripheral sealing, over extensions, are truly significant in prosthetic failure. Not all the modifications suggested by the patient can be made; if they are not possible, the patient or companions are convinced firmly and clearly. Not performing the posterior peripheral seal implies inadequate extension, by not guiding the technician in the posterior delimitation of the prosthesis, gagging reflex in the patient, lack of support to oppose the adhesive force, and pushing in all directions allowing the entry of air, liquids and food between the base and the mucosa. Once the test is satisfactorily completed, the acrylic is processed and the prosthesis is finished. 1.6. Clinical metal testing [18-20].
The metal structure test allows you to check the correct seating of the metal framework in the mouth, whether it is a removable or fixed partial denture. In the removable metal structure, if the seating of the occlusal supports in their respective occlusal beds, the adaptation of the direct and indirect retention units, adaptation and sealing of the major connector in the palatal vault, adaptation and sealing is not checked and achieved well of the major connector in the lower arch, minor connectors, interference of the retention pins for the teeth, as well as the insertion and disinsertion path of the prosthesis that is perpendicular to the occlusal plane, would bring serious difficulties in the completion of the prosthesis.
Therefore, special attention must be paid when assessing the adaptation and adjustment, retention, stability and occlusion of the metal test. The different parts of the metal structure must be carefully reviewed and rejected when there is an absence of a retaining arm, dental or mucosal support, among others. 1.7. Finishing of the prosthesis and revisions [18-21].
It may be the case that the finished prosthesis arrives at the specialist with a note from the laboratory stating one of these situations that occurred during the completion of the prosthesis, suggesting a solution or considering repeating the treatment: Teeth and retainers out of position, fractured, bite lift, porosities (a common defect that can be repaired when it is localized and mild, otherwise a repetition should be indicated for aesthetic reasons and not force the patient to accept the case), stained acrylic, roughness and irregularities in the settling surface, plaster included in acrylic, among the most frequent.
The treatment of the dental prosthesis does not end at the stage of placing the rehabilitative treatment, since, if the necessary adjustments are not made, the patient will not be able to use the prosthesis comfortably, nor will the integration between the patient and the patient be achieved. biological environment.
It is advisable to verify at the molar level that they occlude simultaneously with the antagonists, the presence of exaggerated contacts, interferences with sliding, cause instability to the dental prosthesis, creating a negative predisposition on the part of the patient to the use of the prosthesis [22,23].
It is essential to use the articular paper and the correct inspection of the occlusion and dental articulation, and begin the occlusal adjustment that is completed in subsequent appointments, after the rearrangement of the bases. The check-ups, once the patient already uses the prosthesis, are as important as the previous ones, however, sometimes there are operators who explain to the patient that if there is no problem, the care has been completed, this can result in the patient seeking comfort, “self-touches” the prosthesis inappropriately where he or she feels discomfort or simply stops using it.
No matter the number of controls carried out, these allow for the most detailed adjustments, the instructions are returned to check whether they were understood by the patient, and they must be recorded in writing, especially if it is a geriatric patient or one with hearing problems. The continuous use of prostheses prevents the oral mucosa from receiving the necessary rest due to the tissue changes that the rehabilitation device causes, such as degeneration of the salivary glands and mechanical blockage of the excretory ducts if they are constantly covered, thus reducing secretion. salivary, the pH and the buffering action of saliva, which favors the accumulation of bacterial plaque [1,2,4,25,26].
This is why many researchers attach great importance to the time of daily use and recommend a break between six and eight hours a day, so that the tissues are oxygenated, recovered and the tongue can achieve self-cleaning.

Figure 10: Elderly patient with incorrect maintenance of removable prostheses and their imbalance
Oral pathology associated with the use of removable prostheses. Comprehensive general dentistry treats man as a biopsychosocial being who is influenced by different risk factors, which can act negatively in the appearance and development of a disease. Knowledge of oral pathologies after prosthetic installation affects millions of adults in the world.
This has motivated a real approach to the problem, in relation to the knowledge, perceptions, attitudes, fears and practices of patients. in the family context and in their community. Many patients are not aware of the damage caused by these risk factors and are not able to modify their behavior in this regard. The patient needs to be informed and taught to develop and improve perceptual actions, in addition to other aspects of this complex biopsychosocial process. It is not always explained to the patient that the useful life of their prosthesis is between 5 and 10 years and that it must also be reviewed every 6 months to avoid the appearance and progression of paraprosthetic injuries due to this mechanical device that is a foreign body on the surface. the biological terrain [15,21,22,23].
It should be noted that sometimes we do not have the calmness and psychological capacity to achieve in patients, especially geriatric patients, to make them aware of the necessary rest and hygienic care of the prosthesis.
Sometimes, patients use dental prostheses for between 10 and 20 years or more and present with clinical manifestations such as changes in the vertical dimension, generally greatly reduced. Furthermore, the use of removable prostheses among older adults is a common situation. Partial or total rehabilitation of edentulism with removable prostheses reproduces to a greater or lesser extent the lost functional and aesthetic capacity, but they are responsible for an associated pathology inherent to their use. In fact, it corresponds to the most common pathology of the oral mucosa of older adults, accounting for between 30% and 60% of all possible lesions [24-26].
It has been shown that individuals who permanently use removable prostheses have more injuries than those who use them discontinuously and the importance of guiding patients and caregivers about the advantages of letting the covered mucosa rest is also reported. by the prosthesis during sleep time, in order to allow the tissues to oxygenate, recover and provide the tongue and lips the opportunity to perform self-cleaning action. The elderly, for the most part, downplay oral health and the consequences that systemic diseases and their treatments have on it, which causes a greater increase in drug consumption, causing important alterations such as dry mouth or oral disorders. of the composition of saliva. Today, the necessary and updated knowledge about aging is available, but society in general and the elderly themselves continue to accept the deterioration of the mouth and chewing system as an inevitable process of aging.
The vast majority of patients with dental prostheses have some injury throughout their prosthetic history. The risk factors that influence the appearance are: advanced age, diabetes, smoking, xerostomia, poor oral hygiene, size and extension of the prosthesis, sleeping with the prosthesis and being wearers of old prostheses (more than 5 years) [26-29].
The most common oral pathologies related to the use of removable prostheses are prosthetic stomatitis, candidiasis, traumatic ulcers, angular cheilitis and exophytic formations. Stomatological prostheses constitute a risk factor for developing premalignant and malignant lesions in the oral cavity, especially when associated with continuous use by the patient and poor hygiene.
The misalignment of the prosthetic devices and the fractures of some of their parts lead to the appearance of these injuries, which are generally located in the residual alveolar ridges. To help improve the oral health of the population, it is necessary to educate them so that they discover and recognize the risk factors that affect their health; then medical care will be more effective. It is important to identify patients with more risk factors to provide them with differentiated care. Promotion and prevention activities in primary care make it possible to guide oral self-examination and modify associated habits [29,30].
Prosthetic stomatitis. It is known by several names, such as prosthetic stomatitis, subplaque palatitis or erythematous palatitis and is a lesion of the palate that is defined as an inflammatory, traumatic, chronic, erythematous, usually asymptomatic lesion of the oral mucosa, caused by the surface internal of a complete or partial removable prosthesis. Denture stomatitis mainly affects the older population who use dental prostheses. Various authors, such as Scully., et al., state that the frequency of this pathology occurs between 65 and 70% of patients who use prostheses in the upper jaw.
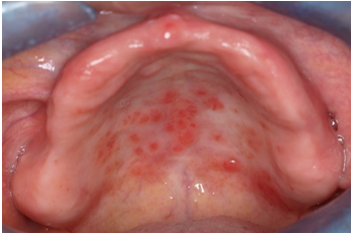
Figure 11: Prosthetic stomatitis in a patient with a removable total prosthesis.
The etiology is of multifactorial origin, related to trauma, duration of use of the prosthesis, poor oral hygiene of the prosthesis, nocturnal use of the same, different species of Candida, material of the prosthesis, permeability of the acrylic resin, immunological factors. and it is also associated with factors secondary to the use of medications such as antibiotics and corticosteroids. Budtz-Jörgensen, in the 1970s, stated that the factor directly related to the formation of the lesion is the colonization of Candida species, specifically Candida albicans as the first to colonize, followed by Candida glabrata, which occupies second place. place of isolated species in cultures of patients with total dentures. The treatment is aimed at eliminating prosthetic trauma as much as possible.
For this, it is usually necessary for the patient to rest from using the prosthesis for between 6 to 8 hours or sleep without it. Adequate oral hygiene of the prosthesis, mainly mechanical, through brushing, is especially important. It can be completed with a chemical cleaning, immersing it in a container with water, to which antiseptic means are added. Old or poorly adapted prostheses will be relined appropriately and if necessary a new one will be made. The treatment of denture stomatitis has been a most discussed topic in the field of oral medicine, with antifungals being the most used for its management.
Exophytic formations. Traumatic removable prostheses can generate pathological growth of lesions such as: - Inflammatory papillary hyperplasia consisting of granulomatous formations caused by the palatal plate of a mucosa-supported upper prosthesis. It can be associated with candidiasis and is asymptomatic. - Fibrous hyperplasia, which consists of a benign exophytic formation, with a polypoid appearance, firmer than the healthy tissue that surrounds it, paler and non-bleeding. - Fissured epulis, this is an exophytic formation located in the alveolar mucosa that consists of the growth of two “V” mamelons that embrace the fin of a removable prosthesis.
Traumatic ulcers. They are tissue losses caused by removable prostheses, frequently due to overextension of the prosthesis and create lesions in the oral mucosa. They are acute, painful from the beginning and with a clear cause-effect relationship. The prosthesis is what defines the injury, the prosthesis must be relieved by trimming and polishing the pressure area. Its disappearance will be confirmed after 15 days and it is not necessary to act on the injury.
Angular cheilitis. It is also known as commissural cheilitis. It is an alteration of the normal trophism of the lip corners with chronic inflammation with nonspecific maceration and fissure with redness, superficial ulceration and crusting in the corners of the mouth extending to the skin. It rarely affects the oral mucosa and can occur unilaterally or bilaterally. Its etiology is variable and is due to four factors such as mechanical (loss of vertical dimension), systemic diseases such as vitamin deficiencies, dermatitis, and fungal and bacterial infectious agents. In older people it is usually due to several factors simultaneously.
In relation to prostheses, it appears when there is a loss of vertical dimension due to old and poorly fitting prostheses. It is usually superinfected by candida, whether or not associated with erythematous palatitis, and hypovitaminosis or malnutrition is not uncommon. It is a more or less painful injury, with a certain degree of functional disability, because the crusted fissures open easily with oral movements. The treatment is aimed at eliminating the causal factors, restoring the vertical dimension, administering the deficient vitamin or nutritional factor and treating the candidiasis with antifungal creams.

Figure 12: Angular cheilitis.
Bone deformities. Bone deformities are also a risk factor in relation to misalignment and damage to the subprosthetic mucosa. In this sense, mandibular and maxillary tori, hypertrophic tuberosities, prominent oblique lines, among other deformities of the dental ridges and alveoli, should be be taken into account. The mandibular or palatine torus are bony excrescences, which can interfere with the patient's physiological functions, as well as with the prosthetic adaptation if required, which is why excision of the torus is recommended.
This surgical act may present a certain degree of complexity or can be very traumatic. As its growth is slow and asymptomatic it is not perceived by patients, it is commonly diagnosed when the patient requires a dental prosthesis. If the torus is large in size, it usually makes the patient uncomfortable due to the presence of constant traumatic ulcerations because the membrane that covers it is extremely thin. Another problem reported is usually the packing of food remains, resulting in halitosis, when the exophytic lesion is large size can alter the physiology of phonation, swallowing and chewing.
Fixed prosthesis on teeth.
As long as the required conditions exist, it is in the interest of both the patient and the professional, when finding edentulous spaces, to prefer rehabilitation using a fixed prosthesis, to restore occlusal functionality in addition to aesthetics, which can offer a better quality of life to the patient.
In order to carry out these types of rehabilitation, patient training, conservation of other dental diseases and carrying out a good diagnosis with a good treatment plan and excellent patient rehabilitation are required. It is known that this fixed prosthesis, once installed, cannot be removed by the patient; and it can only be done by the dentist with the application of appropriate techniques and the use of specific instruments. However, it has the danger of deterioration of the prosthesis and the possibility of causing trauma to the abutment tooth where it is located. The assessment of the abutment teeth is essential for the success of a fixed prosthesis treatment on teeth. Molars are preferable as abutments because they have more than one root over single-rooted teeth. Tilted teeth will be avoided because they prevent conventional carving and jeopardize the viability of the long-term treatment.
For a multi-piece fixed prosthesis on teeth to be successful, two requirements must be met. The first of these is that the surface of the abutment teeth They must be equal to or greater than that of the supported teeth and that the crown-root ratio (considering the beginning of the root and the alveolar crest) is 2:3 and the minimum valid is 1:1, otherwise the restorations will be compromised. in the short and long term.

Figure 13: Premolar prepared to receive a ceramometallic crown.

Figure 14: Metal test of the crown in the previous image.
The healthy relationship between dental restorations and the periodontium is of utmost importance for the clinical and aesthetic harmony of the restorations, it includes the adaptation with the periodontal tissues, a diagnosis and planning of the case, in addition to correct periodontal and prosthetic clinical execution. To rehabilitate a tooth using an intraradicular fixed partial prosthesis, prior treatment of the root canals through endodontics is required; Therefore, it is necessary to perform confirmatory x-rays to verify not only the periodontal conditions, but fundamentally the status of the pulpo-radicular treatment, because a poorly prepared canal can be the cause of failure of the rehabilitative treatment to be performed.
To determine that the root treatment is correct, the following factors must be considered: Type of material used in endodontics, it must be gutta-percha, because materials such as silver points can generate lateral perforation. Maintain a good seal at the apical level. Eliminate the smallest amount of dentin from the root canal and thus avoid the weakening of the root walls and ensure the resistance of the canal so that the treatment has a better prognosis, always taking into account the thickness necessary to be able to place an intraradicular post.
There are risks that increase the potential for tooth fracture after endodontic treatment. Due to the loss of the tooth structure and the subsequent endodontic treatment, the walls of the canal thin after instrumentation, which makes the tooth more susceptible to fracture, the progressive destruction of enamel and dentin; determining factor for the fragility of the remaining dental tissue.
Regarding the design of the fixed prosthesis restoration, both biological and mechanical elements must be considered, such as the biological space, the contour and the contact point.
Effective endodontic treatment and root apical sealing are essential aspects to allow the installation of intraradicular retainers. However, placing an intraradicular post does not strengthen or reinforce the tooth; These properties are given by the residual dental structure and the surrounding alveolar bone, the post must jointly accompany the bending of the dental tissues against loads; Therefore, they should not be placed indiscriminately but only in cases that warrant it, such as; teeth that have been endodontically treated and with considerable loss of crown tissue. Short intraradicular posts (posts) can cause tooth fractures, and improper shape can cause a wedge effect. The diagnosis of occlusion must be rigorously managed when using ceramic materials such as crowns and pontics, maintaining occlusion as a group, relieving contact points to maintain functional occlusion and avoiding overfilling.
Fracture resistance is related to roots weakened by excessive wear of the canal walls and the trigger effect that the post can produce in the canal.
Fixed prosthesis on implants. Implantology is not free of risks, so it is necessary to anticipate its appearance whenever possible. Fortunately, the percentage of complications that occurs is minimal at 3.8%. To minimize this result, correct individual planning for each patient is essential. There are a series of parameters that lead to the appearance of complications that in turn lead to the appearance of clinical failures, such as

Figure 15: Poor planning of a single prosthesis treatment on implants.
Mechanical problems with fixed implant prostheses are the most common complications that occur in dental treatments with implants. These may be fundamentally due to forces resulting from functional or parafunctional movements that exceed the adaptive capacity of the system. Various studies divide mechanical complications into
Mechanical complications entail greater expense for patients and a loss of perceived quality. Avoiding these complications is a challenge for the industry and for the restoration professional.
Dental practice, in its beginnings, was not exempt from confrontations with clinical situations that gave rise to erroneous diagnoses, deficient or incorrect treatment planning until a change was achieved in its philosophy towards an interdisciplinary and multidisciplinary attitude in treatments from the emergence of the different disciplines.
With interdisciplinarity, higher quality of health services is achieved, with better results for the population, providing minimum risk and adequate use of available resources to execute preventive-curative actions in dentistry.1 The discipline of Stomatological Prosthetics, which emerged in 1968, establishes an interrelationship as an integral part of the therapeutic plans in pediatric patients with the disciplines of Orthodontics, Periodontics and Surgery; The great development in the different current materials and techniques2 contributes to its improvement; from a community model to improve the quality of dental care and the degree of satisfaction with the services received.
Within Stomatology, interdisciplinary planning of dental treatment is essential to ensure its success, since each discipline fulfills its role and all complement each other.
The use of prostheses to replace prematurely lost teeth is very interesting in pediatric dentistry.
In the last forty years, numerous articles have been published on the subject; however, its clinical application is relatively new4. It is considered that if earlylife,oss is not replaced in pediatric patients, there is a significant psychological impact, since the patient is deprived of an important part of their own identity and may suffer maladjustment, impacting their psychosocial well-being and therefore in their quality of life, so the specialist must take extreme care, show admiration, empathy, and inspire confidence in the work done and perceived by the parents and the child or adolescent themselves.
Therefore, pediatric rehabilitation must consider, in addition to an adequate clinical and laboratory treatment plan, the psychological aspect, and for effective care it is necessary to take into account the criteria of a multidisciplinary team from the initial approach6. With prosthetic treatment, the coronary portions or the replacement of early lost teeth and their associated parts can be adequately replaced by artificial means capable of restoring the masticatory, aesthetic and phonetic function; which is why it acquires a therapeutic character, in addition to restoring the anatomy of one or more teeth and the relationship between the jaws of the patients.
It is recommended to take extreme care when this treatment is performed on children or adolescents, and once the desired dental correction is obtained, or the causal factor of tooth loss is eliminated, the prosthodontist must perform his or her part of the rehabilitative treatment using provisional prostheses, the re-evaluation, and subsequently the creation of definitive prostheses at the appropriate time.
The restoration of extracted teeth, using removable or fixed prostheses, benefits different physiological functions; such as, for example, phonation, swallowing, chewing and renewal of lost aesthetics. It is difficult for pediatric patients to manage them as they feel like a foreign body in continuity or contiguity with the contact tissues within the oral cavity. If a harmonious relationship is established, the response of the subjects is good, it depends on the characteristics of the prosthesis, the way and capacity of the tissues to react, the actions and knowledge of the basic principles for its construction, the careful attention to the technique used to reduce possible aggression or keep it within acceptable biological limits.
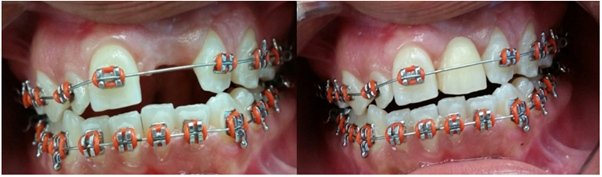
Figure 16: Restoration of the upper central incisor in an adolescent patient.
The decision to use any type of prosthesis should be based on clinical experience, good judgment, the availability of appropriate prosthetic materials, knowledge of the growth and development phases of the pediatric patient and the principles of occlusion, age and characteristics of the patient who will receive it.
The removable prosthesis in children provides a temporary service; It will replace temporary teeth until the permanent ones erupt or it will replace young permanent teeth, until the patient reaches the appropriate age to receive a fixed prosthesis.
The use of prostheses to replace prematurely lost teeth in children is one of the most interesting parts of pediatric dentistry, for this reason and the risks involved in any therapeutic error at this stage of life, it is a topic that deserves special attention. attention. Furthermore, the dentist who is going to design and construct dental prostheses for these patients must have adequate knowledge about the growth and development of the dental arches, dentition and occlusion, eruption sequence and chronology of the dentition, otherwise, there is a risk that the effect, far from being beneficial, will be deleterious, and the consent of the patient and his guardian could not be obtained.
Prosthetic rehabilitation is a specialty in which different dentomaxillofacial anomalies are treated, where each treatment can present multiple risks and complications that will affect the quality of life of the patients and their expectations would be affected.
To my wife and my children, thank you God for blessing my family.
Copyright: © 2024 Otto Alemán Miranda., et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
ff
© 2024 Acta Scientific, All rights reserved.